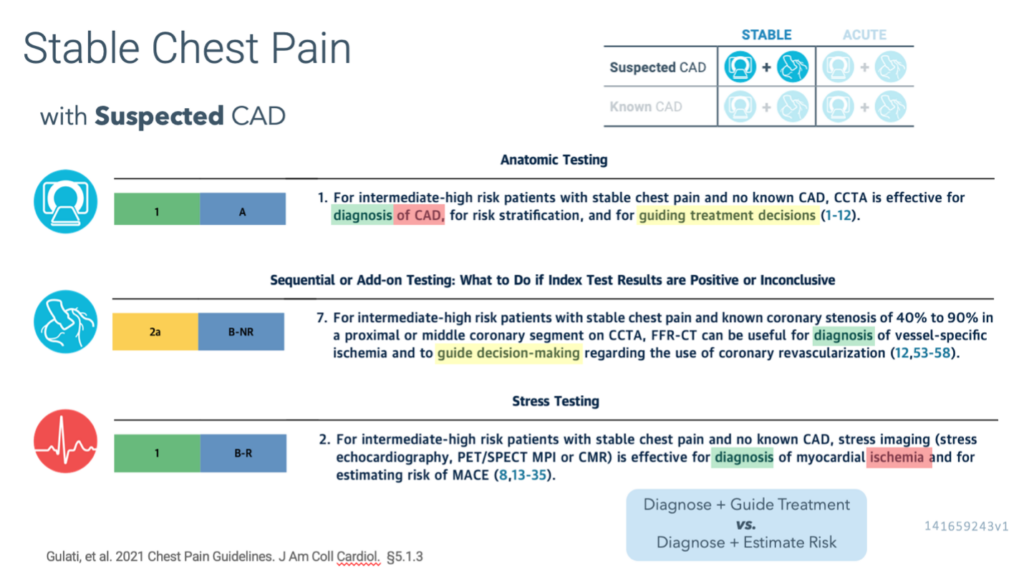
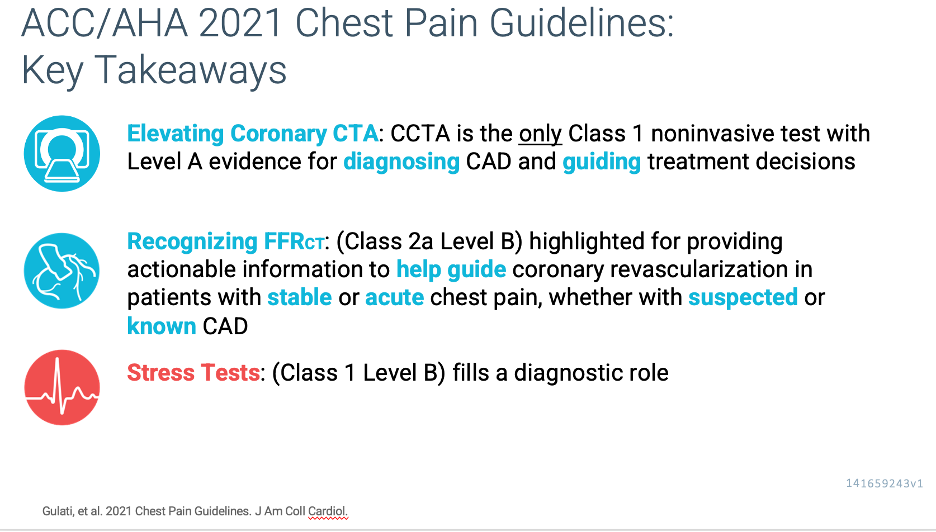
Coronary CTA as a class I Level of Evidence A for diagnosing and treatment guidance of CAD in intermediate and high-risk patients with no known CAD.
Although it is well known that guideline-based recommendations are evidence based, the evidence used to support the use of cardiac imaging has traditionally been limited, as prior data evaluating the clinical effectiveness of imaging have mostly focused on diagnostic accuracy rather than on the impact of testing on patient management and outcomes.
However, over the past decade, the quantity and quality of evidence supporting various clinical indications for noninvasive testing have grown substantially, especially for new imaging techniques.
Consequently, the new guideline was based on a comprehensive and critical evaluation of the contemporary evidence base in imaging. Priority was given to randomized controlled clinical trials that evaluated patient outcomes.
The guidelines state that “for intermediate risk patients with acute chest pain and no known CAD who are eligible for cardiac testing, either exercise electrocardiography, stress echocardiography, stress PET/SPECT MPI, or stress CMR is useful for the diagnosis of myocardial ischemia” (Class 1; LOE: B, nonrandomized), whereas “CCTA is useful for exclusion of atherosclerotic plaque and obstructive CAD” (Class 1; LOE A). Among patients with acute chest pain, invasive angiography is recommended (Class 1; LOE C, expert opinion) in the presence of moderate to severe ischemia on a current or prior (≤1 year) stress test, or in the presence of high-risk CAD (left main ≥50% or 3-vessel ≥70% stenosis), or obstructive CAD (≥50%) and frequent angina. Invasive angiography is also suggested as an option if there is moderate to severe ischemia on an imaging stress test or abnormal fractional flow reserve–computed tomography (FFR-CT) imaging after coronary computed tomography angiography (CTA) with inconclusive stenosis or obstructive CAD.
Implications for Imagers
Imagers and clinicians need to be selective in deciding who requires further testing and avoid testing in those who are unlikely to benefit from additional investigations. Intermediate-risk patients may benefit from further noninvasive testing. Similarly, as described earlier, CAC testing in low-risk individuals and a contemporary pretest probability model of obstructive CAD can be used to identify stable patients in whom testing may be deferred. In fact, when evaluating the pretest probability of obstructive CAD table (Figure 11 in the guideline), all women aged <60 years and all men aged <40 years would be expected to have a pretest probability <15%. When testing is believed to be required in such low-risk patients, calcium scoring or exercise treadmill testing (both Class 2a) may be options for the index evaluation.
Imagers also need to promote effective use of testing by ensuring that unnecessary test layering is avoided. Clinicians should use the initial test results and severity and frequency of symptoms to intensify guideline-directed medical therapies and guide the need for follow-up testing.
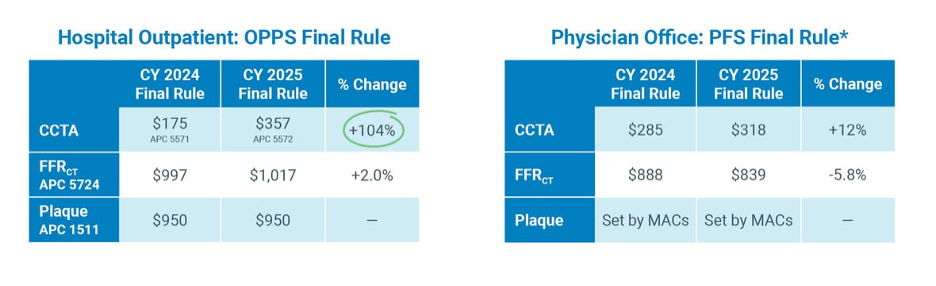
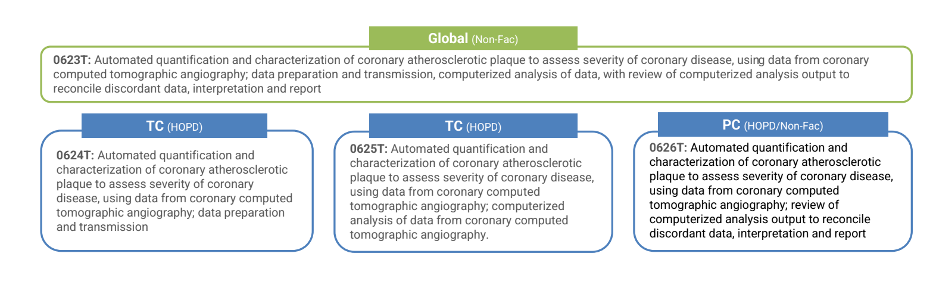
Imagers need to be familiar with the strengths and limitations of different imaging approaches to ensure appropriate selection of the best test. In keeping with this principle, it is important to recognize the advantages of newer testing options (eg, plaque detection or FFR-CT imaging on coronary CTA [3], higher diagnostic accuracy and quantitative assessment of myocardial blood flow with PET, use of CMR for suspected myocardial infarction with nonobstructive coronary arteries). The recommendations of this and other guidelines are based on the available scientific data, rather than on local availability or economic factors. It is thus expected that evidence-based recommendations should ultimately drive clinical practice patterns and payment, rather than the other way around.
FFR-CT imaging is suggested as a testing option following coronary CTA in patients with both stable and acute chest pain when there is 40% to 90% stenosis in a proximal or mid-vessel (Class 2a). Furthermore, coronary CTA and stress test options are presented for evaluating patients with various manifestations of nonobstructive plaque, a clinical entity that is increasingly common.